If you’ve experienced extended pelvic pain, you’re not alone. As many as 15 to 20 percent of women between the ages of 18 and 50 will experience chronic pelvic pain that lasts six months or more. Pelvic pain can have many causes and sometimes it’s difficult to find a specific cause.
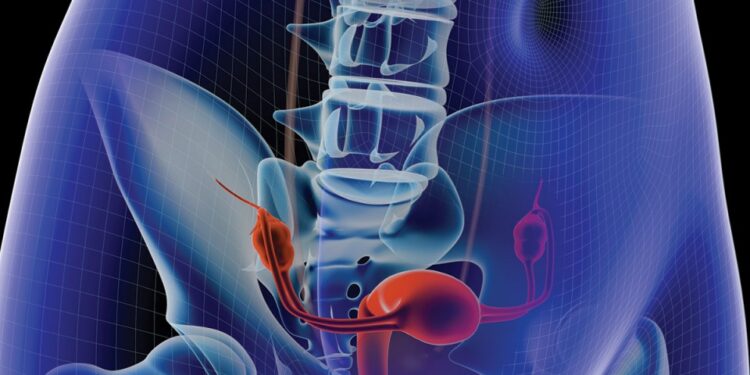
It is estimated that approximately 70 percent of these women will have endometriosis, a painful disorder in which tissue that normally lines the inside of your uterus—the endometrium—grows outside the uterus, or anywhere else where it’s not supposed to grow. It usually grows on the ovaries, the fallopian tubes, the outer wall of the uterus, the intestines, or other organs in the abdomen or pelvis.r
r
“The problem with endometriosis is that it can be difficult to diagnose.”r—Ginny Ripley, family practitioner at Nebraska Methodist Health System
r
rThe condition becomes troublesome when the displaced tissue continues to act as it normally would if it was inside the uterus and continues to thicken, break down, and bleed with each menstrual cycle. However, because the tissue is outside of the uterus, the blood cannot flow outside of the body. The displaced tissue can build up around the affected area and can become irritated, resulting in scar tissue, adhesions, or fluid-filled sacs called cysts. For women in their childbearing years, the adhesions may block the fallopian tubes and cause infertility.
“The problem with endometriosis is that it can be difficult to diagnose,” says Ginny Ripley, family practitioner at Nebraska Methodist Health System. “It doesn’t show up in ultrasounds or CAT scans, so the only definitive way to get a diagnosis is through surgery. Surprisingly, we’ve found that the severity of a woman’s symptoms do not correlate to the severity of the condition.”
So while some women with extensive endometriosis may have no symptoms at all, others may experience painful periods, heavy periods or bleeding, pelvic pain during ovulation, and pain during bowel movements or urination. The pain is usually located in the abdomen, lower back, or pelvic areas. Many women don’t realize they have endometriosis until they go to the doctor because they can’t get pregnant, or if they have a procedure for another problem. It is estimated that 20 to 40 percent of women who are infertile have endometriosis.
Because of the difficulty in diagnosing endometriosis, it is often a matter of ruling out other causes first before arriving at a diagnosis of endometriosis, notes Dr. Ripley. Other common causes of pelvic pain include fibroids, chronic pelvic inflammatory disease caused by long-term infection, pelvic congestion syndrome, an ovarian remnant, irritable bowel syndrome, interstitial cystitis, and musculoskeletal factors.
The type of treatment a woman receives will depend on the severity of symptoms and whether or not she is planning to become pregnant. Several treatments have to be tried before it is determined what works best. Many women can be treated successfully with anti-inflammatories or a combination of anti-inflammatories and oral contraceptives and/or hormone therapy. Anti-inflammatories help reduce bleeding and pain. Birth control pills and hormone therapy help shrink the endometrial tissue by lowering hormone levels and help suppress the growth of additional endometrial implants—but they also prevent pregnancy.r
r
“While the tissue growth may come back, it often cleans up the area long enough to allow a woman to conceive.”r—Katherine Finney, M.D., obstetrician/gynecologist University of Nebraska Medical Center
r
rIn more severe cases in which all other options have been exhausted, surgery may be recommended to remove the extra tissue growth, says Katherine Finney, M.D., obstetrician/gynecologist at the University of Nebraska Medical Center. Surgery is performed laparoscopically. This means that the doctor places a small, lighted tube through a small incision in your belly and looks for signs of displaced endometrial tissue. The tissue can then be removed or destroyed through heat or cauterization.
“While the tissue growth may come back, it often cleans up the area long enough to allow a woman to conceive,” says Dr. Finney. “Rates of conceiving are higher after surgery, but some women may still need fertility treatments to help as well.”
If pregnancy is not a goal, medications, such as hormone therapy, can be taken following surgery to prevent the growth of new or returning endometriosis, says Dr. Finney.
For women with severe pain due to endometriosis, a hysterectomy may be considered as a last option; however, this is rarely needed anymore. “We do far fewer hysterectomies today than we have in the past because we have so many other effective options,” says Dr. Ripley.
Some women may not require treatment, as they have no or only mild symptoms, while others can have notable symptoms due to pain and/or infertility issues. Treatment is typically based on symptoms. If you are near menopause, you may want to consider managing your symptoms with medications rather than surgically. Once you stop having periods, endometriosis will usually stop causing you problems, notes Dr. Finney. In rare cases, post-menopausal women will still experience continued pain, in which case their physician should evaluate them to determine if they are a candidate for surgery.